Many of our patients come to us with some fictional assumptions of typical symptoms of sleep apnea, ways to treat it and some false expectations of CPAP therapy. Some people are going off friends’ experiences, myths on the internet or their limited experience with CPAP treatment. Therefore, this blog will go over common myths we hear from our patients and provide factual answers as well as informative and proven advice on diagnosing and effectively treating Sleep Apnea and Obstructive Sleep Apnea (OSA).
First we’ll start with myths about sleep apnea: the condition, the symptoms, who are prone to be diagnosed, and how to treat it. Our next blog will feature myths specifically about CPAP Treatments.
MYTH #1: Everyone that Snores had Sleep Apnea

This is not true. While snoring is often associated with Obstructed Sleep Order (OSA). Not all snorers have OSA, for example, those who are in the obese weight category may be more prone to snoring. Also, snoring can be a result of such factors that include: the anatomy of your mouth and sinuses, alcohol consumption before sleeping, allergies, a cold, or your weight.
If your snoring is accompanied by other risk factors of OSA, such as excessive daytime sleepiness, poor concentration, irritability especially in children, high blood pressure, sore throat upon wakening, and snoring so loud you disrupt your partner’s sleep, then you should talk to your physician.
The only way to truly diagnose sleep apnea is a sleep study or sleep apnea test called a polysomnogram (PSG). A polysomnogram (also called a sleep study) is a multiple-component test that electronically sends and records specific physical activities while you sleep. The recordings are analyzed by a qualified sleep specialist to find out if you have sleep apnea or another type of sleep disorder. Only a medical practitioner or physician can officially diagnose your condition and prescribe treatment.
MYTH #2: If I Lose Weight, My Sleep Apnea will be Cured
While studies have shown that there is a strong link between excess weight and sleep apnea, it’s not the only risk factor that can contribute to OSA. Even those of average weight and under weight can still suffer from a Sleep Related Breathing Disorder. Why is weight a contributing factor of OSA? People who are overweight are more likely to have extra tissue in the back of their throat, which can fall over the airway and block the flow of air into their lungs while they are sleeping. However, losing weight can yield improvements in sleep apnea symptoms.
“If overweight and obese people lose weight, it would make both sleep apnea and other health problems [such as heart disease] go away. Losing just 10% of body weight can have a big effect on sleep apnea symptoms. In some cases, losing a significant amount of weight can even cure the condition.”
– Harvard Health Publishing, Harvard Medical School

If one of our patients has a significant decrease (or increase) of weight, they may need an adjustment in their pressure settings or may need to repeat a Titration Study for an accurate modification to their CPAP settings. (The pressure settings can only be adjusted by a medical practitioner’s prescription.)
So, while its always a good idea to lose weight (if you’re overweight), exercise regularly, cut out fatty and sugary foods, and replace with healthier options (fruits, vegetables, lean proteins and hearty grains), it may or may not alter your OSA symptoms, nor your need to continue your CPAP treatment.
*Never discontinue CPAP treatment without first consulting your medical practitioner and/or DME supplier. Our skilled and certified staff at Everything CPAP is adept at navigating you through various changes in your health, weight and CPAP settings, and will advise you to speak to your physician when needed.
MYTH #3: Only Men Have Sleep Apnea
This is obviously not true, as we have a good percentage of female CPAP patients. The increased prevalence among men as well as the more prominent symptoms of male patients have probably led to this particular myth. “Sleep apnea occurs in about 25% of men and nearly 10% of women“, according to the Cleveland Clinic (March 2020). The Mayo Clinic agrees with this,
“Men are two to three times more likely to have sleep apnea than women.” (July 2020)
– Mayo Clinic
Women’s risk increases if they are overweight or they have completed menopause, as the risk increases for both men and women as they get older. Symptoms in men get more attention as well, because they commonly complain of snoring, gasping, snorting and apnea; while women’s common symptoms include headache, fatigue, depression, anxiety and sleep onset insomnia. When a partner complains of hearing snoring through the night, men are more prone to address and treat their symptoms.
“Higher prevalence of obstructive sleep apnea (OSA) in men compared to women has been consistently reported by previous clinic-based and community-based studies. In addition, OSA is more severe in men compared with women matched for body mass index, although this sex difference decreases with increasing age.”
– Journal of Thoracic Disease, May 2019
Regardless of gender, those who suffer with OSA need to get treatment as the risk factors go beyond snoring, daytime fatigue, and poor concentration, for example, among the most serious comorbidities of sleep apnea are stroke, diabetes, heart disease and even potentially cancer.
MYTH #4: Drinking Alcohol makes me Sleep Better
It’s easy to assume that generally alcohol not only relaxes you but helps you sleep better. The drink’s affect on your sleep though becomes less successful over time, so while a significant amount of alcohol will help you fall sleep, it will not help you stay asleep through the night. Alcohol reduces the amount of REM sleep, the stage of sleep where your eyes move rapidly (giving this stage its name) and is vital for your health. Why is REM sleep important?

“REM sleep plays a significant role in helping your brain consolidate and process new information. This information is then retained in your long-term memory. REM sleep also helps to ensure better mental concentration and mood regulation.”
– The National Sleep Foundation
Alcohol can actually put you at a greater risk of OSA, especially if you have an alcohol use disorder; and for those with OSA, alcohol can worsen symptoms and present dangerous complications. According to VeryWellHealth.com, “Studies show that moderate or heavy drinking can cause episodes of obstructive sleep apnea in people who don’t even have the condition.”
Why it’s dangerous to mix alcohol and OSA:
- The effects of alcohol can increase the time between when you stop breathing and ‘wake up’ to breath again.
- Alcohol can cause a drop in your blood’s oxygen level, called desaturation, which can lead to increased carbon dioxide in your body, which in severe cases can be fatal.
- Alcohol decreases your drive to breath, slowing your breathing and making your breaths shallow, which can contribute to your upper airway to collapse, increasing snoring and can interfere with your CPAP treatment.
MYTH #5: Only Adults have Sleep Apnea
Again, this is an easy myth to disprove, since a percentage of our patients are children from infancy to 18 years old. In fact, according to a 2019 study published in the Journal of Osteopathic Medicine, between 7 and 11 percent of children have a nighttime breathing disorder, whether it’s sleep apnea, snoring, or something else. Around 90 percent of them may be undiagnosed.
While some pediatric symptoms may be more indicative a potential risk of OSA and more easy to recognize for parents (like snoring, pauses in breathing, coughing or choking while sleeping), other symptoms may be harder to link to OSA, including:

- Bedwetting
- Sleeping in odd positions
- Sleep terrors
- Irritability and daytime sleepiness
- Restlessness during sleep
- Learning problems including difficult paying attention in school, or ADHD
- Morning headaches
- A Nasal voice
- Need for napping past the age of napping
- Mood disorders
- Growth and cognitive delays
- Heart problems
Just like adults, if you suspect a child may be suffering with OSA, the first step is seeing your doctor or pediatrician. For proper diagnosis, the doctor will ask about your child’s symptoms, perform a physical examination and schedule a sleep study, if needed.
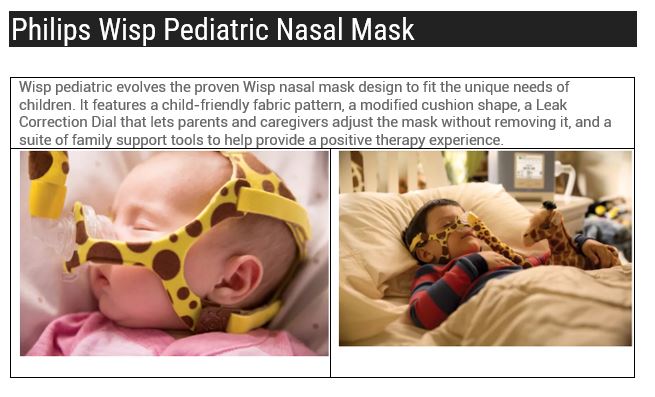
For treatment in pediatric patients, it can begin with lifestyle changes, nasal steroids, oral appliances and in severe cases, tonsil surgery. More than likely, your child may need CPAP therapy and there are several pediatric options developed for them in recent years, including a choice of Pediatric CPAP Masks made for children of various age groups: including infants weighing at least 22 pounds to 7 years old, as well as mask sized for children above 7 years old to young adults.
Everything CPAP has experience conducting fittings and trainings for our pediatric patients, with ongoing support as the child grows. We do our best to make the experience as fun and relaxing for our little ones, as well as providing guidance and training for their parents and guardians. Our goal for parents and children, of a certain age, is to show the importance of compliance and persisting through the adjustment period.
“As in adults, compliance with PAP therapy is a key factor in determining success. Adolescents pose a particular challenge. For many children, however, the dramatic improvement in the way they feel … becomes an important motivating factor.”
– The American Sleep Apnea Association
Our mission at Everything CPAP is help child and parent get comfortable with CPAP, show parents how to implement CPAP as their nightly routine, making needed adjustments and training to help them stick with it, and encouraging children to keep the masks on throughout the night. We offer various pediatric mask options including:

Our next blog will feature additional Myths-versus-Facts regarding CPAP Treatment including:
- MYTH #6: CPAP Treatment cures Obstructive Sleep Apnea
- MYTH #7: CPAP Treatment is Uncomfortable & Difficult to Use
- MYTH #8: CPAP Therapy is Expensive
- MYTH #9: CPAP Treatment is a One-Size-Fits-All System
- MYTH #10: There is Insufficient Ongoing Support & Help with your CPAP Treatment, after your Initial Trial Period
- MYTH #11: I Could Suffocate if the Power Goes Out (with a Full Face Mask)
- MYTH #12: Utilizing CPAP Treatment makes me Unattractive
If you suspect you or your child may be suffering from OSA, take our online quiz and Get Started on a Better Night’s Sleep: